Promoting Palliative Care in Heart Failure Pilot: The P3HF Study
Grant # R34HL174885
02-September-2024 to 30-June-2027
Heart failure is a leading cause of morbidity and mortality, projected to affect over eight million Americans by 2030. Patients often experience frequent symptoms, hospitalizations, and readmissions, particularly near the end of life, yet fewer than 20% receive Specialist Palliative Care despite strong recommendations from key organizations like the American Heart Association. A key factor for referral is patient prognosis. Our team developed and validated a 1-year mortality risk model embedded into an electronic health record (EHR)-based alert to support clinician decision-making. While the model was accurate and feasible, it did not significantly increase referrals to palliative care, likely due to its interruptive nature, leading to clinician overrides. To address this, we propose designing and piloting the Promoting Palliative Care for People with Heart Failure (P3HF) clinical decision support (CDS) tool, integrating the mortality risk model with evidence-based CDS design and implementation strategies. The project will involve interviews, iterative design, and focus group evaluations to ensure the tool’s usability and feasibility. A real-world pilot trial will assess its impact on clinician behavior (primary outcome: palliative care referrals) and patient outcomes (e.g., advance care planning, hospice enrollment, hospital readmission rates). The results will inform a multi-site clinical trial, aiming to improve palliative care delivery and quality of life for heart failure patients.

Evaluation of the Yale New Haven Health System Mortality Surprise Question: Clinician Perspectives
Grant # P30AG021342
Claude D. Pepper Center Pilot Program.
Dates 7/102024-6/30/2025
The goal of this mixed methods study is to evaluate the implementation and outcomes of the Mortality Surprise Question initiative across the Yale New Haven Health System.
Identifying Successful Strategies of Specialist Palliative Care Implementation for People with Advanced Heart Failure
Grant # R01HL172840
15-September-2024 to 30-June-2027
Each year, over 280,000 people in the U.S. die from advanced heart failure, facing severe symptoms, frequent hospitalizations, and delayed transitions to hospice care. Despite clinical guidelines recommending palliative care to address these challenges, fewer than 20% of patients with advanced heart failure receive specialist palliative care. This gap underscores the need for better understanding of the structures and processes that enhance the reach and effectiveness of palliative care in this population.
Our proposal aims to address these gaps by identifying the key modifiable factors that contribute to high-reach palliative care and improved end-of-life outcomes. Specifically, we focus on increasing days spent at home, promoting hospice enrollment ≥ 7 days before death, and improving family-reported end-of-life care quality. To achieve this, we will conduct a multisite, mixed-methods study within the Department of Veterans Affairs (VA), the largest healthcare system in the U.S. with an integrated electronic health record system. This allows us to assess both VA and Centers for Medicare and Medicaid data to examine end-of-life care inside and outside the VA.
Through quantitative and qualitative analyses, we will identify successful strategies used by medical centers that have effectively implemented specialist palliative care for advanced heart failure. Our findings will provide actionable insights for expanding and improving palliative care delivery nationwide, ultimately enhancing patient and family experiences at the end of life.
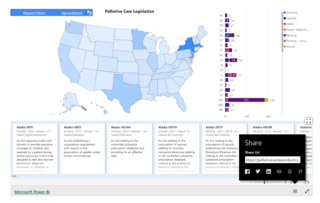
The Palliative Care GPS
In the U.S., there are growing efforts to improve access to palliative care through state-level advocacy, with many new policies emerging. The Solomon Center for Health Law and Policy at Yale Law School, along with the Center to Advance Palliative Care (CAPC), launched a platform called the Palliative Care Law and Policy GPS in 2021 to track palliative care legislation across all 50 states. The platform gathers data on laws and bills related to palliative care from 2010 to the present.
The project focuses on seven key areas:
- Clinical Skill-Building: Laws that improve healthcare professionals’ ability to communicate with patients and offer symptom relief, including training in palliative care, pain management, and advance care planning.
- Payment: Policies that ensure funding for palliative care services, such as Medicaid benefits or insurance coverage for palliative care.
- Pediatric Palliative and Hospice Care: Laws that promote the development of pediatric palliative care programs, benefits, and workforce training.
- Public Awareness: Efforts to increase the public’s understanding of palliative care, such as public campaigns and informational resources.
- Quality/Standards: Laws that set quality measures and standards for palliative care, such as defining palliative care and tracking outcomes like location of death and use of hospice.
- Telehealth: Policies that expand access to palliative care through telemedicine, including changes to reimbursement and face-to-face visit requirements.
- Workforce: Laws that support the growth of the palliative care workforce, such as certification programs or loan forgiveness for palliative care professionals.
This initiative helps track and promote progress in improving palliative care access and quality across the country.
The GPS aims to:
- Offer a detailed, current overview of state-level palliative care policy.
- Enable analysis of how policies differ across the U.S.
- Track legislative trends in palliative care.
- Identify gaps in legislation and highlight successful policy solutions.
- Promote innovative policy approaches.
- Encourage policy development, particularly in underserved communities.
Completed Projects
RePORT ⟩ RePORTER
Grant # R56HL166523
Dates 9/1/2023-8/30/2024
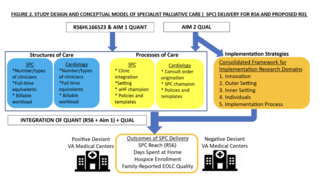
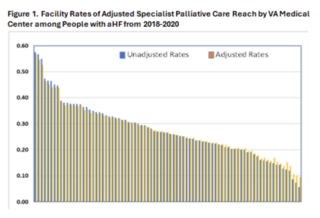
Over 280,000 people die from advanced heart failure each year in the United States. This population experiences burdensome symptoms, frequent hospitalizations, and delayed transitions to hospice care. Clinical practice guidelines recommend the use of palliative care for persons with advanced heart failure to address this population’s many palliative care needs. However, nationally the uptake of specialist palliative care remains low, and implementation across hospitals varies widely, limiting effectiveness. As hospitals move to implement specialist palliative care into clinical practice for persons with advanced heart failure, there is little evidence to guide them as to what components are necessary or how to implement this care. Without such information, the uptake of specialist palliative care will remain low thereby contributing to poor care at the end of life. Our proposed project will address these critical knowledge gaps. Our long-term goal is to increase the low uptake of specialist palliative care and to improve end-of-life care quality among people with advanced heart failure. As a step towards this goal, the objective of this proposal is to identify modifiable factors and implementation strategies that medical centers can use to develop specialist palliative care programs for this population, beginning in the Department of Veterans Affairs (VA). The VA is the largest healthcare system in the United States and is the only healthcare system whose integrated electronic health record supports a rigorous and comprehensive evaluation of specialist palliative care delivery involving features of both palliative and cardiology practices. To accomplish our objectives, we will use a multisite, sequential, explanatory mixed methods design and a positive deviance approach. We will evaluate associations between specialist palliative care and cardiology program composition (i.e., structures) and operational characteristics (i.e., processes) and the uptake of specialist palliative care (Aim 1) and important outcomes of end-of-life care quality including hospice enrollment before the last seven days of life, and family-reported end-of-life care quality (Aim 2). We will accomplish these aims using a novel dataset comprised of patient and hospital-level data from 83 VA medical centers, detailed data on structures and processes of specialist palliative care and cardiology programs, and surveys of bereaved family members combined with Medicare and Medicaid claims. Next, we will compare structures, processes, and implementation strategies across twelve medical centers by conducting interviews with specialist palliative care and cardiology clinicians, and through the analysis of policy documents and consultation templates (Aim 3). We will integrate quantitative and qualitative data (Aim 4) to identify strategies that facilitate the effective delivery and implementation of specialist palliative care for persons with advanced heart failure. This proposal directly aligns with NOT-HL-20-737 by identifying real-world, pragmatic strategies that address barriers and facilitate sustained delivery of specialist palliative care. Findings from our project can inform and refine specialist palliative care programs nationwide for persons with advanced heart failure.
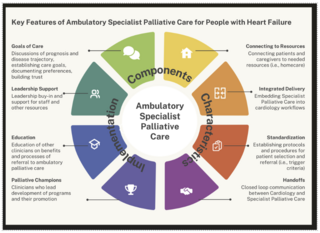
Exploring Patient, Family-Caregiver, and Clinician Perspectives of Outpatient Models of Palliative Care Delivery
Grant #: NINR 5U2CNRO14637 (Feder Project PI)
Dates 7/1/2021-6/30/2022
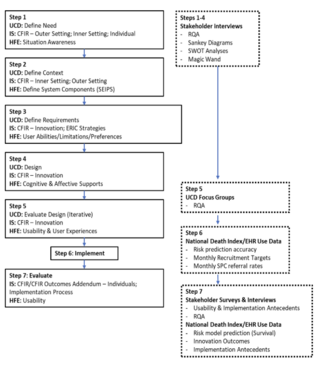
This project was a mixed methods study designed to identify key components, structures and processes, and strategies for implementation in promoting timely outpatient palliative care for people with heart failure.